Fistula for Dialysis
Overview
Vascular Access for Hemodialysis
A vascular access is a hemodialysis patient’s lifeline, because it makes life-saving hemodialysis treatments possible. Hemodialysis is a treatment for kidney failure that uses a machine to send the patient’s blood through a filter, called a dialyzer, outside the body. The access is a surgically created vein used to remove and return blood during hemodialysis. The blood goes through a needle, a few ounces at a time. The blood then travels through a tube that takes it to the dialyzer. Inside the dialyzer, the blood flows through thin fibers that filter out wastes and extra fluid. The machine returns the filtered blood to the body through a different tube. A vascular access lets large amounts of blood flow continuously during hemodialysis treatments to filter as much blood as possible per treatment. About a pint of blood flows through the machine every minute. A vascular access should be in place weeks or months before the first hemodialysis treatment.
Two types of vascular access designed for long-term use include the arteriovenous (AV) fistula and the AV graft. A third type of vascular access—the venous catheter—is for short-term use.
What is an arteriovenous fistula?
An AV fistula is a connection, made by a vascular surgeon, of an artery to a vein. Arteries carry blood from the heart to the body, while veins carry blood from the body back to the heart. Vascular surgeons specialize in blood vessel surgery. The surgeon usually places an AV fistula in the forearm or upper arm. An AV fistula causes extra pressure and extra blood to flow into the vein, making it grow large and strong. The larger vein provides easy, reliable access to blood vessels. Without this kind of access, regular hemodialysis sessions would not be possible. Untreated veins cannot withstand repeated needle insertions, because they would collapse the way a straw collapses under strong suction.
Health care providers recommend an AV fistula over the other types of access because it
- Provides good blood flow for dialysis.
- Lasts longer than other types of access.
- Is less likely to get infected or cause blood clots than other types of access.
Before AV fistula surgery, the surgeon may perform a vessel mapping test. Vessel mapping uses Doppler ultrasound to evaluate blood vessels that the surgeon may use to make the AV fistula. Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital. A radiologist—a doctor who specializes in medical imaging—interprets the images. The patient does not need anesthesia for this procedure. A Doppler ultrasound shows how much and how quickly blood flows through arteries and veins so the surgeon can select the best blood vessels to use.
A surgeon performs AV fistula surgery in an outpatient center or a hospital. The vascular access procedure may require an overnight stay in the hospital; however, many patients go home afterward. A health care provider uses local anesthesia to numb the area where the surgeon creates the AV fistula.
An AV fistula frequently requires 2 to 3 months to develop, or mature, before the patient can use it for hemodialysis. If an AV fistula fails to mature after surgery, the surgeon must repeat the procedure.
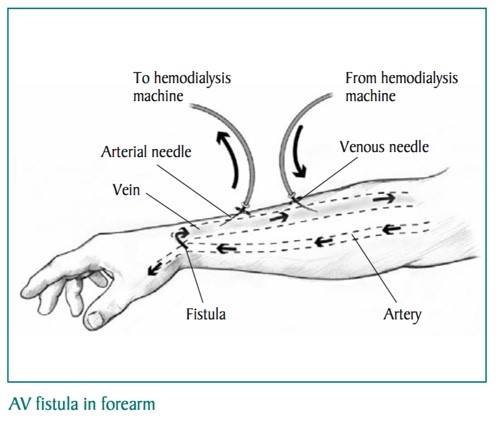
At the start of a hemodialysis session, a health care provider or the patient inserts two needles into the vascular access. One needle carries blood from the body to the dialyzer. The other carries filtered blood back to the body. To tell the needles apart, the needle that carries blood away from the body is called the arterial needle. The needle that carries blood back to the body is called the venous needle. Some patients prefer to insert their own needles into the vascular access, which requires training to learn how to prevent infection and protect the vascular access. No matter who inserts the needles, the patient should know how to take care of the needle insertion area to prevent infection.
If an AV fistula does not mature, an AV graft is the second choice for a long-lasting vascular access.
What is an arteriovenous graft?
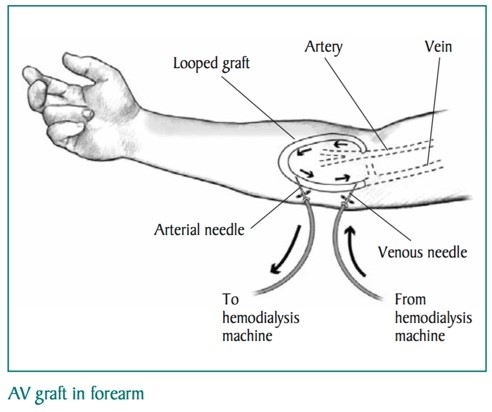
An AV graft is a looped, plastic tube that connects an artery to a vein. A vascular surgeon performs AV graft surgery, much like AV fistula surgery, in an outpatient center or a hospital. As with AV fistula surgery, the patient may need to stay overnight in the hospital, although many patients can go home after the procedure. A health care provider uses local anesthesia to numb the area where the surgeon creates the AV graft.
A patient can usually use an AV graft 2 to 3 weeks after the surgery. An AV graft is more likely than an AV fistula to have problems with infection and clotting. Repeated blood clots can block the flow of blood through the graft. However, a well-cared-for graft can last several years.
A patient can usually use an AV graft 2 to 3 weeks after the surgery. An AV graft is more likely than an AV fistula to have problems with infection and clotting. Repeated blood clots can block the flow of blood through the graft. However, a well-cared-for graft can last several years.
Set Up the Vascular Access Well before Starting Hemodialysis
Patients should set up a vascular access well before starting hemodialysis, as AV fistulas and AV grafts both need time to mature before they are ready for use. A health care provider can help schedule an appointment with a vascular surgeon well before the patient starts hemodialysis, even if the patient is feeling fine. Giving a vascular access time to mature can help prevent problems with narrow veins, low blood flow, and blood clots.
Before the procedure, health care providers should use the back of the patient’s hand for drawing blood to preserve the blood vessels in the arm. A health care provider can teach the patient simple exercises that help the blood vessels grow larger for the surgeon’s use. The same exercises help the AV fistula grow larger after the procedure.
Before the procedure, health care providers should use the back of the patient’s hand for drawing blood to preserve the blood vessels in the arm. A health care provider can teach the patient simple exercises that help the blood vessels grow larger for the surgeon’s use. The same exercises help the AV fistula grow larger after the procedure.
What is a venous catheter?
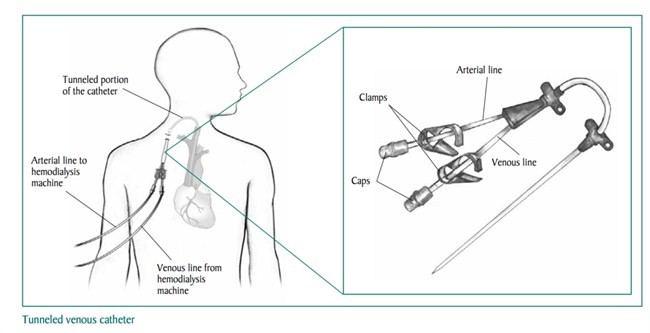
A venous catheter is a tube inserted into a vein in the neck, chest, or leg near the groin, usually only for short-term hemodialysis. The tube splits in two after the tube exits the body. The two tubes have caps designed to connect to the line that carries blood to the dialyzer and the line that carries blood from the dialyzer back to the body. A person must close the clamps on each line when connecting and disconnecting the catheter from the tubes.
If kidney disease has progressed quickly, a patient may not have time for placement of an AV fistula or AV graft before starting hemodialysis treatments.
A nephrologist—a doctor who specializes in kidney problems—or an interventional radiologist—a doctor who uses medical imaging equipment to perform operations—performs the venous catheter placement procedure in a hospital or an outpatient center. The patient receives local anesthesia and sedation to stay calm and relaxed during the procedure.
Venous catheters are not ideal for long-term use. With a venous catheter, a patient may develop a blood clot, an infection, or a scarred vein, causing the vein to narrow. However, if a patient needs to start hemodialysis right away, a venous catheter will work for several weeks or months until a surgeon can perform a long-term access surgery and the AV fistula or AV graft has time to mature.
If fistula or graft surgery is unsuccessful, then a patient will need a long-term venous catheter access. When a patient needs a venous catheter for more than 3 weeks, the surgeon will “tunnel” the catheter under the skin, rather than insert it directly into the vein. A tunneled catheter is more comfortable and has fewer problems. Even tunneled catheters, however, may become infected.
What problems could a vascular access cause?
All three types of vascular access—AV fistula, AV graft, and venous catheter—can cause problems that require further treatment or surgery. The most common problems include access infection and low blood flow due to blood clotting in the access.
Infection and low blood flow happen less frequently in properly formed AV fistulas than in AV grafts and venous catheters. Still, having an AV fistula does not guarantee the access will be problem-free.
AV grafts more often develop low blood flow, an indication of clotting or narrowing of the access. The AV graft may then require angioplasty, a procedure to widen the narrow part. Another option involves surgery on the AV graft to replace the narrow part.
Venous catheters are the most likely to cause infection and clotting problems. If these problems develop, medication may help. Antibiotics are medications that fight bacteria that can cause infection. Blood thinners such as warfarin keep blood from clotting. If these treatments fail, a nephrologist or an interventional radiologist will need to replace the catheter.
How does a patient care for and protect a vascular access?
A patient can care for and protect a vascular access by:
- Ensuring that the health care provider checks the access for signs of infection or problems with blood flow before each hemodialysis treatment, even if the patient is inserting the needles.
- Keeping the access clean at all times.
- Using the access site only for dialysis.
- Being careful not to bump or cut the access.
- Checking the thrill in the access every day. The thrill is the rhythmic vibration a person can feel over the vascular access.
- Watching for and reporting signs of infection, including redness, tenderness, or pus.
- Not letting anyone put a blood pressure cuff on the access arm.
- Not wearing jewelry or tight clothes over the access site.
- Not sleeping with the access arm under the head or body.
- Not lifting heavy objects or putting pressure on the access arm.
Eating, Diet, and Nutrition
Researchers have not found that eating, diet, and nutrition play a role in causing or preventing problems with a vascular access.
More information about eating well during hemodialysis is provided in the NIDDK health topic, Eat Right to Feel Right on Hemodialysis.
Kidney stones that are too large to pass on their own or cause bleeding, kidney damage or ongoing urinary tract infections may require more-extensive treatment. Procedures may include:
Points to Remember
Besides the questions you prepare in advance, don’t hesitate to ask any other questions during your appointment as they occur to you.
- A vascular access is a surgically created vein used to remove and return blood during hemodialysis.
- An arteriovenous (AV) fistula is a connection, made by a vascular surgeon, of an artery to a vein.
-
Health care providers recommend an AV fistula over the other types of access because it
○ Provides good blood flow for dialysis.
○ Lasts longer than other types of access.
○ Is less likely to get infected or cause blood clots than other types of access. - An AV graft is a looped, plastic tube that connects an artery to a vein.
- A venous catheter is a tube inserted into a vein in the neck, chest, or leg near the groin, usually only for short-term use.
- Venous catheters are not ideal for long-term hemodialysis. With a venous catheter, a patient may develop a blood clot, an infection, or a scarred vein, causing the vein to narrow.
- All three types of vascular access can cause problems that require further treatment or surgery. The most common problems include access infection and low blood flow due to blood clotting in the access.
Emergency Cases
Please feel welcome to contact our friendly reception staff with any general or medical enquiry call us.
Opening Hours
Monday – Friday 8.00 – 7:00 pm
Saturday 9.00 – 8.00 pm
Sunday 10.00 – 9.00 pm